Can Periodontal Disease Make Your Diabetes Worse?
Can Treating Periodontal Disease Make Your Diabetes Better?
Does diabetes affect the bacteria in your mouth? And can the bacteria in your mouth make it harder to control your blood sugar? Scientists and dentists say, “Yes!” Even though dentists have been aware of the connection between periodontal disease and diabetes for many years now, this knowledge hasn’t been communicated very well to you and me. In this article I will show you what scientists have learned about how periodontal disease can make your diabetes worse. It should be great motivation to take your at-home dental care seriously.
For people with diabetes, the connections go both ways. Bad bacteria in the mouth actually make it harder to control blood sugar. And hyperglycemia (high blood sugar) contributes to the growth of bad bacteria in the mouth. So, poor blood sugar control and poor oral hygiene form a negatively reinforcing cycle of bad health.
A Look at Periodontal Disease
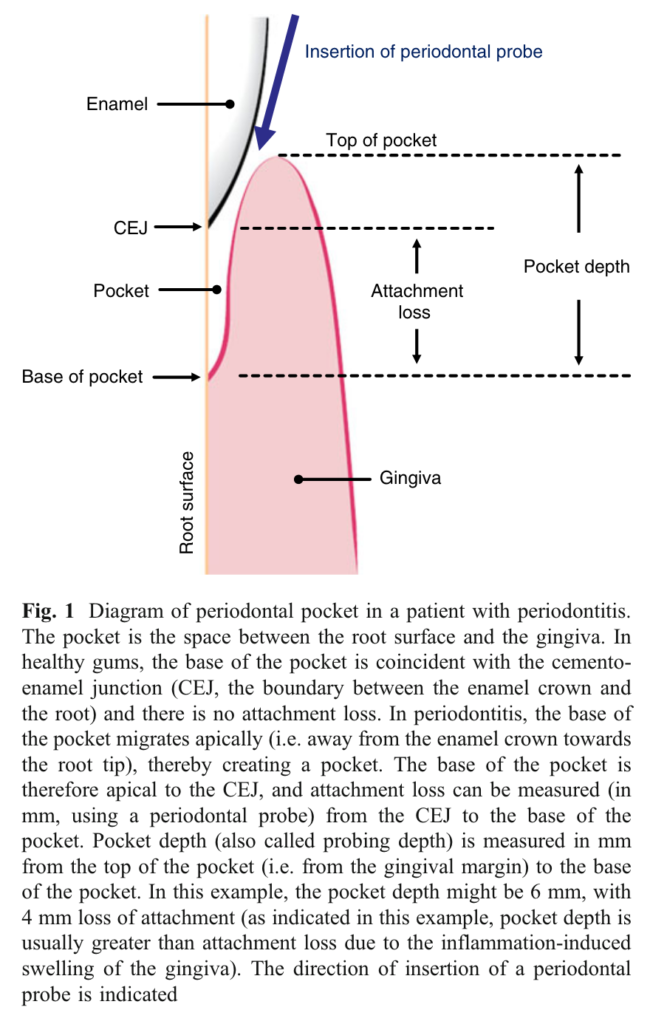
We don’t appreciate the dangers of pathogenic bacteria in the mouth very well. We know we should brush out teeth to avoid cavities. But we don’t think of our overall health when it comes how brushing our teeth, flossing, and making sure we clean along the gum line . A figure from this study is given here to help you visualize what periodontal disease is all about. A healthy pocket should stop at the cementum-enamel junction (CEJ). But pathogenic bacteria in plaque set up a biofilm along the gumline. This causes inflammation and starts a war with your immune system. As a result of this inflammation a periodontal pocked is formed with the gum tissue pulled away below the CEJ along the root surface.
Periodontal Disease is Very Common
Periodontal diseases are more common than we think. In the general population 10-15 percent of adults have severe periodontitis. They have it so severe that they are in danger of losing all their teeth. And moderate periodontitis affects 40-60 percent of the population. This is great news if you are a dental hygienist, as you will never run out of work. But if you are on the receiving end of that dental care, you had better pay attention!
Smoking is a risk factor for getting periodontitis. So is any condition which compromises your immune system, like osteoporosis, some medications, genetics, and diabetes. Obesity and low physical activity are risk factors for periodontitis. But you already know that obesity and being sedentary are risk factors for every disease known to mankind, so that isn’t big news to you.
Diabetes is a Risk Factor for Periodontal Disease
People don’t generally know that diabetes is a risk factor for periodontal disease. Do people suffering with diabetics have to also worry about losing their teeth, along with their eyesight, their fingers and toes, kidney failure, heart disease, hearing loss, Alzheimer’s disease, and possibly pancreatic cancer, liver cancer and colorectal cancer? The health outlook for diabetics is not good. (I have a lot more to say about reversing diabetes elsewhere. Just know for now that it is possible for most people to reverse their diabetes. They certainly can severely limit the negative health outcomes of runaway, uncontrolled diabetes. And I’m not talking about the next “miracle drug” coming down the pipeline.)
Article: Diabetics have 3-Fold Higher Risk of Periodontal Disease
In an article that was written as a result of the European Workshop in Periodontal Diseases and Diabetes that was held in London, on 26 May 2010, it was stressed that inflammation from periodontal disease, and inflammation from diabetes negatively reinforced each disease process. The authors noted that diabetics had a three-fold higher risk of periodontitis compared to the general population. As noted above, about half of the general population has moderate periodontal disease. This means that virtually every diabetic person is at high risk of gum disease and severe periodontal disease.
And diabetics with severe periodontitis had about a 3-fold higher risk of dying from heart disease or kidney failure compared to diabetics without severe periodontitis. So, good oral hygiene is an essential part of conquering diabetes.
Are all diabetics at risk? What if someone is a diabetic but has no signs or symptoms of any oral disease? Are they at risk?
Even “Healthy” Diabetics Are at Higher Risk of Periodontal Disease
A recent study answered just such a question. It turns out that diabetics with no oral disease at all still have altered populations of bacteria in their mouth and higher concentrations of metabolites that don’t normally occur in healthy people. More periodontal pathogens like Porphyromonas gingivalis and Prevotella melaninogenica are more common in diabetics even without signs of gum disease. And metabolites like cadaverine (sounds nasty whatever it is) and n,n-dimethylarginine were present in significantly higher amounts, indicating dysregulation of metabolism in the mouth. So, there is indeed increased risk of periodontitis if you have diabetes but no oral disease…yet.
It has long been thought that inflammation was the connection between periodontitis and diabetes. And it definitely is one key link, but new research has shown that the story is a bit more intriguing. Science is always limited by what can be measured. The instruments to measure are always a key part of new scientific discoveries.
Oral Bacteria can Become Gut Bacteria by Translocation
It is now possible to use DNA and RNA sequencing as well as protein sequencing to analyze particular strains of bacteria. See, even within a particular genus and species of a bacteria there are strains that are benign and strains that are absolutely pathogenic. Take, for example the E. coli O157:H7 strain. Many strains of E. coli are benign and commensal, living peacefully within us. But the E. coli O157:H7 can cause bloody diarrhea and can lead to hemolytic uremic syndrome, which is very dangerous, even deadly in young children and the elderly.
The point is that the particular strain of a bacteria is very important. So, now scientists are able to detect particular strains from the oral cavity and the colon and see if they match. If it is the same strain, then the bacteria in the colon came from the mouth, survived the mouth-gut barrier, and colonized in the small and large intestine.
By use of meta‑genomic, transcriptomic, and proteomic analyses of paired saliva and stool samples collected from 35 individuals from 8 families with multiple type 1 diabetics (17 of them actually) a research group at the University of Luxembourg found that the lower abundance of Streptococcus salivarius in the mouth was correlated with lower abundance of this beneficial bacteria in the gut. In the mouth there were more Streptococcus mutans, rather than S. salivarius, which survived the more acidic environment in type 1 diabetics caused by low production of saliva and higher glucose concentration in their saliva. And these differences in the mouth were reflected in the relatively low concentrations of S. salivarius in the gut of the diabetic subjects as well.
Translocation of Oral Bacteria to Gut Bacteria is More Common in Diabetics
So, it is becoming more clear that some oral bacteria do indeed survive the mouth-gut barrier of stomach acid and bile secretions and go on to colonize in the small and large intestine. If the bacteria are pathogenic in the mouth, they will also be pathogenic in the gut. Another study, similar to the one I talked about in a recent blog, found ectopic (out of place) colonization of bacteria in the colon. In healthy people they saw less than 0.9 percent of the bacteria in the colon with their origin being the mouth. But in type 2 diabetic patients they found that the rate was 2.36%, more than twice as high as healthy people. So, some colonization appears to be normal, but in a chronic inflammatory state like diabetes there are more pathogenic bacteria in the mouth, and a compromised gut as well that seems easier to be colonized by pathogenic bacteria.
So, the increase of pathogenic bacteria in the gut is bad news for people with diabetes. These bacteria continue to cause inflammation and contribute to declining health in diabetics. And more systemic inflammation leads to easier colonization of the mouth by even more pathogenic bacteria. The inflammation in the gut makes it harder for the immune system in the mouth to get the upper hand against the pathogenic bacteria that have made the periodontal pockets their home. It is a downward spiral that requires serious intervention.
Treatment of Periodontal Disease Improves Blood Sugar Control in Diabetics
Now, researchers have proven over and over that people with diabetes and periodontitis that undergo professional care for their oral infection can improve their glycemic control. A meta-analysis found that about 4 months after a professional cleaning and treatment of their periodontitis there was a drop in HbA1c of 0.4 percent, which is clinically significant.
Action Points to Break the Negative Spiral of Periodontal Disease and Diabetes
So, what can we take away as action points from all of these scientific findings?
Be Aware of 3-fold Greater Risk
First, diabetics need to be aware of their greater risk of periodontal disease, with about 3-fold higher risk of negative health outcomes and irreversible tissue loss in the gums and cementum layer that holds their teeth in their sockets. Loss of teeth from periodontal disease is a very real possibility for type 2 diabetics. That thought alone should move you to action.
You Must Manage Diabetes and Oral Health at the Same Time
Second, diabetics must manage their glucose levels and oral health at the same time. Bad oral bacteria tend to worsen glycemic control, and uncontrolled hyperglycemia leads to the growth of bad oral bacteria. It is a negative interactive cycle with dire consequences.
Gum Health is as Important as Tooth Health
Third, gum health is a very important part of oral hygiene. Products like Ora-Shield are very beneficial for gum health, as the essential oils in this 100% organic blend have strong effects in helping balance the beneficial bacteria and potentially pathogenic bacteria in the mouth, including the bacteria in gingival crevices. By reducing the populations of periodontal bacteria, you can reduce the inflammation in the gingival crevices, which can lead to healing of that microenvironment and lower pocket depths and healthier gums. This in turn leads to better glycemic control.
Toothpaste is great for reducing dental cavities in teeth, but gum health may take more work. If toothpaste worked so well, there probably would not be much of an issue with gum disease. But gum disease is a huge issue, so we need more help. Consider incorporating Ora-Shield into your oral hygiene routine and say hello to fresh breath and a healthy mouth.



Pingback: Unlock Wholesome Gums with a Water Flosser – GetResult